|
St John of God Hospital in Warrnambool welcomed the Stryker Mako robot in 2023. Mr Sutherland has been trained on the use of the robot, in Victoria, NSW, and also in the UK, and began using the robot to assist with knee replacement in July 2023.
Robotic knee replacement surgery offers several advantages for individuals suffering from knee problems. Firstly, the precision of robotic assistance allows surgeons to tailor the procedure to each patient's unique anatomy, resulting in better alignment and fit of the new knee implant. This can lead to improved function and longevity of the replacement joint. Additionally, robotic technology enhances the surgeon's ability to remove damaged tissue with minimal impact on surrounding healthy structures, leading to faster recovery times and reduced post-operative pain. Overall, robotic knee replacement surgery offers patients a more accurate, less invasive, and faster recovery option for restoring mobility and relieving pain in their knees. The western diet and the tendency to obesity are involved in a lot of problems of the musculoskeletal system. Excess weight bears down on joints and the extra fat tissue carries an additional inflammatory load, further straining joints and other organs. Obesity is also associated with greater risks when people have joint replacement surgery. All of this means that orthopaedic surgeons are quite interested in helping patients to achieve weight loss. There are many approaches to weight loss but, as the graphic below stresses, there are pitfalls and structure to the process is important. In particular there is the old adage that you "cannot outrun a bad diet" - the calories that you put in are always more important than exercise to burn them off, particularly if sore joints limit your ability to exercise.
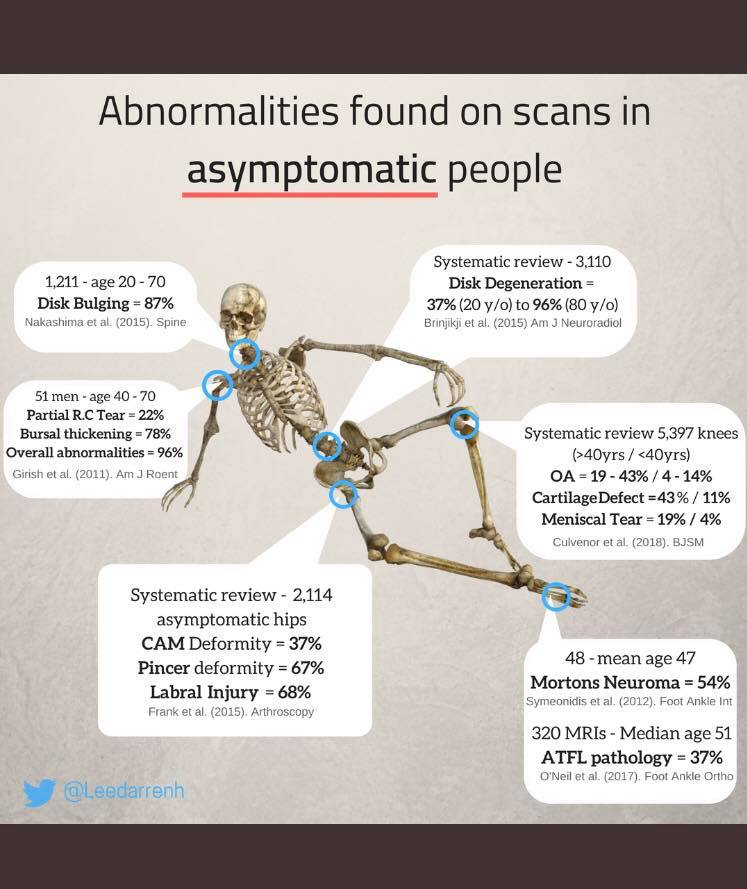
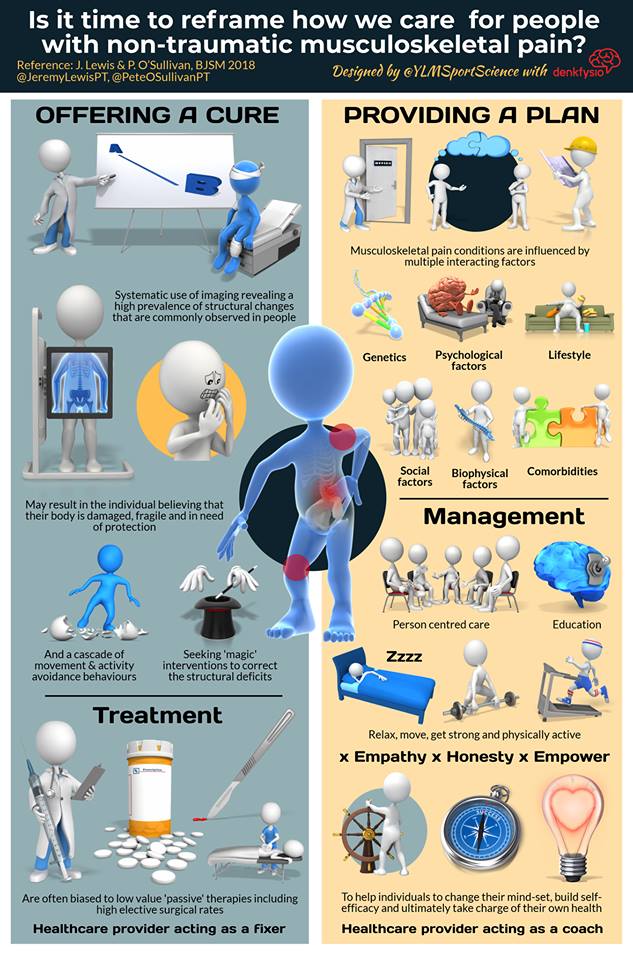
See Renaissance Periodization for further information. It is all too easy to respond to a patient's complaints with a referral for a scan. A 70 year old with knee pain might have a meniscus tear, but they are also more likely to have osteoarthritis (in which case the meniscus tear is irrelevant).
It is the old approach: take a history, examine the patient, use investigations to clarify the differential diagnosis options. A good doctor sometimes says no, but the sensible patient also sometimes turns down an opportunity to get diagnosed or treated Is this really necessary? What are the risks? Are there other options? What happens if I don’t do anything? Christer Mjåset Patients often come with an expectation that the doctor will sort out their problems, with a simple pill or a simple operation. People often say to me that they "don't like taking pills" and would rather have an operation to sort the problem; this demonstrates that a lot of people underestimate the risks associated with surgery. We are, to a degree, victims of the success of modern medicine.
Sometimes the longest, hardest consultations involve explaining why I don't have an operation to fix the problem. But even if we are considering surgery, we still have to go through a proper consent process that incorporates and expands Dr Mjaset's 4 questions: What are we treating? Are there other options, what happens if I don’t do anything? What does the operation involve? What is the aftermath of the operation like? What are the risks? Is this the right thing to do? This good TED talk discusses this at more length. I actually don't see this as a re-framing - it is how I was taught to practice .
My old Professor, Jimmy Hutchison always urged us to seek non-surgical options first - "there is nothing that you can't make worse by operating on it". I can't speak for other surgeons around the country. I choose to use the same hip and knee replacements for all of my patients, private and public. That choice is made on the long-term published results of those replacements.
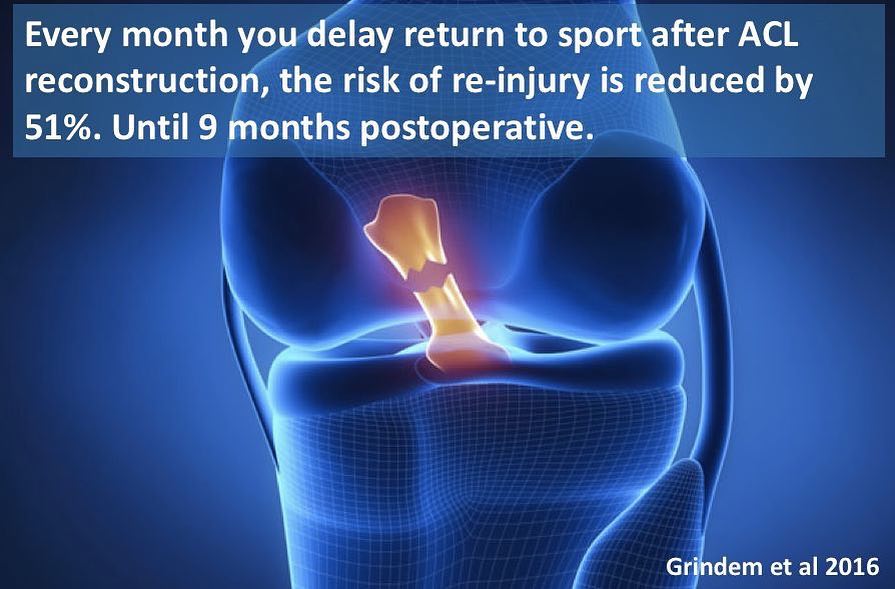
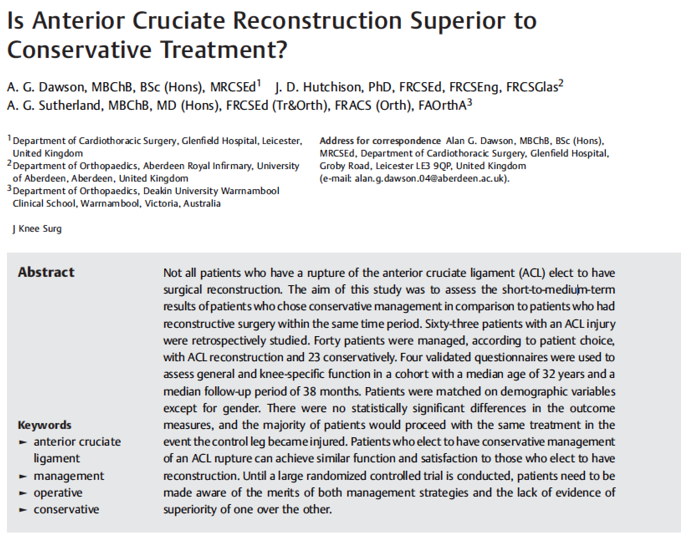
Choose the best equipment available and get consistent at using it well for the best long term results.  click here to see the original article: Warrnambool Standard I feel a bit like a “stuck record”, although this is an analogy that younger people might not understand. Maybe a “GIF” stuck on repeat. Anyway. Here we go again, let me say it once more: The indication for ACL reconstruction is not "ACL injury". Rather, the reason for a patient having an ACL reconstruction is "instability after ACL injury, in spite of a period of good rehab". So, there is actually nothing different about Karen’s approach. This is how I have treated ACL injuries for years. And about ⅔ of the patients that I see with ACL injuries end up having surgery. So, not everyone, but it still has a place when rehab doesn’t quite get the patient where they want to be. This is supported by a paper that I co-authored some years ago (the patients were all under my care), published in the Journal of Knee Surgery: Is anterior cruciate reconstruction superior to conservative treatment?
A Dawson, JD Hutchison, AG Sutherland. J Knee Surg 2016; 29(1): 74-9. I’m slightly surprised that St John of God Warrnambool should support an article that only shows one side of the discussion, but there you go. If you have an ACL injury, you should start rehabilitation with an experienced physiotherapist early. You should discuss your progress and your goals. You should also consider a discussion with a surgeon who regularly treats ACL injuries, about the practicalities and goals of surgery. Some people do really well with rehab, and go back to sports. Some people do well enough with rehab, but decide not to go back to sports. But some people want to go back to sports but cannot because the knee is still unstable, or the knee is still unstable in daily activities, despite good rehab. Those are the people who should consider ACL reconstruction. So many shades of grey. Of course, the answer is "yes". Still very much needed ("kneeded"? Ha Ha).
What this review ACTUALLY says is this: The indication for ACL reconstruction is not "ACL injury". Rather, the indication for ACL reconstruction is "instability after ACL injury, in spite of a period of good rehab" Which is how I have treated ACL injuries for years. And about ⅔ of the patients that I see with ACL injuries end up having surgery. So, very much still needed, just not by everyone. You can read the full review here www.physio-network.com/acl-surgery-no-longer-kneeded/ It goes both ways! In this excellent article, the remarkable Atul Gawande delves into the impact of computers in healthcare, sharing his experience and exploring some of the alternatives. Gawande is a smart man, and a very perceptive writer, and his books are well worth a read, particularly "Complications" and "Better".
|
AuthorAlasdair Sutherland produces Blog updates aimed at patients and general practitioners, to discuss matters of interest and information relating to orthopaedic issues. Archives
May 2024
Categories |
|






 RSS Feed
RSS Feed
